Choosing a Specialist Doctor can be tough. Pain often prevents you from doing what you need or love to do.
Orthopaedics is a medical specialty that deals with the treatment of bones and muscles. Orthopedic surgery is the branch of medicine concerned with diseases, injuries, and conditions of the musculoskeletal system relating to the body's muscles and skeleton. This includes the joints, ligaments, tendons, and nerves.
Orthopaedic surgeons are devoted to the prevention, diagnosis, and treatment of disorders of the bones, joints, ligaments, tendons and muscles. Some orthopaedists are generalists, while others specialize in certain areas of the body, such as: Hip and knee. Foot and ankle.
M.B.S.S. Ortho Med Clinic, is Specialised in Bone & Joint Care situated in Villivakkam which is within easy reach of everybody

Dr. B. Pasupathy
We the M.B.S .S. Ortho in simple; provide compassionate, patient-focused orthopedic care to help you get back to doing what you love. With our expertise rehabilitative care, we offer comprehensive orthopedic care. Dr. B.Pasupathy is an Orthopedic Surgeon in Villivakkam, Chennai. He has an experience of 30 years in this field. He completed MBBS from Thanjavur Medical College in 1990, MS - Orthopaedics from Madras Medical College, Chennai in 2002 Diploma in Orthopaedics from The Tamil Nadu Dr. M.G.R. Medical University (TNMGRMU) in 1996. He is a member of Indian Orthopaedic Association. Dr. B. Pasupathy, M.B.B.S, M.S. Orth., D. Orth., DNB Orth., MNAMS, is a Consultant Orthopaedic, Arthroscopic Surgeon. He did Arthroscopy Fellowship from Germany, Paediatric Sports Injury from Boston Children Hospital, Harvard University, USA. He is a Professor of Paediatric Orthopaedics, ICH & HC in Madras Medical College, Chennai, 2011-2017. Presently he is working as Professor of Orthopaedics, Madras Medical College, Chennai.
M.B.S.S Ortho Med
Our Doctor is Specialised in the following Treatments
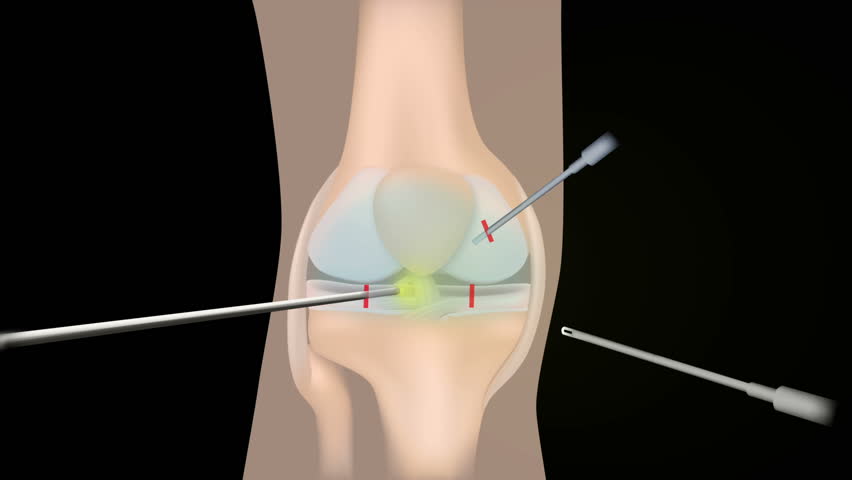
Arthroscopy (also called arthroscopic or keyhole surgery) is a minimally invasive surgical procedure on a joint in which an examination and sometimes treatment of damage is performed using an arthroscope, an endoscope that is inserted into the joint through a small incision. Arthroscopic procedures can be performed during ACL reconstruction. The advantage over traditional open surgery is that the joint does not have to be opened up fully. For knee arthroscopy only two small incisions are made, one for the arthroscope and one for the surgical instruments to be used in the knee cavity. This reduces recovery time and may increase the rate of success due to less trauma to the connective tissue. It has gained popularity due to evidence of faster recovery times with less scarring, because of the smaller incisions. Irrigation fluid is used to distend the joint and make a surgical space. The surgical instruments are smaller than traditional instruments. Surgeons view the joint area on a video monitor, and can diagnose and repair torn joint tissue, such as ligaments. It is technically possible to do an arthroscopic examination of almost every joint, but is most commonly used for the knee, shoulder, elbow, wrist, ankle, foot, and hip.
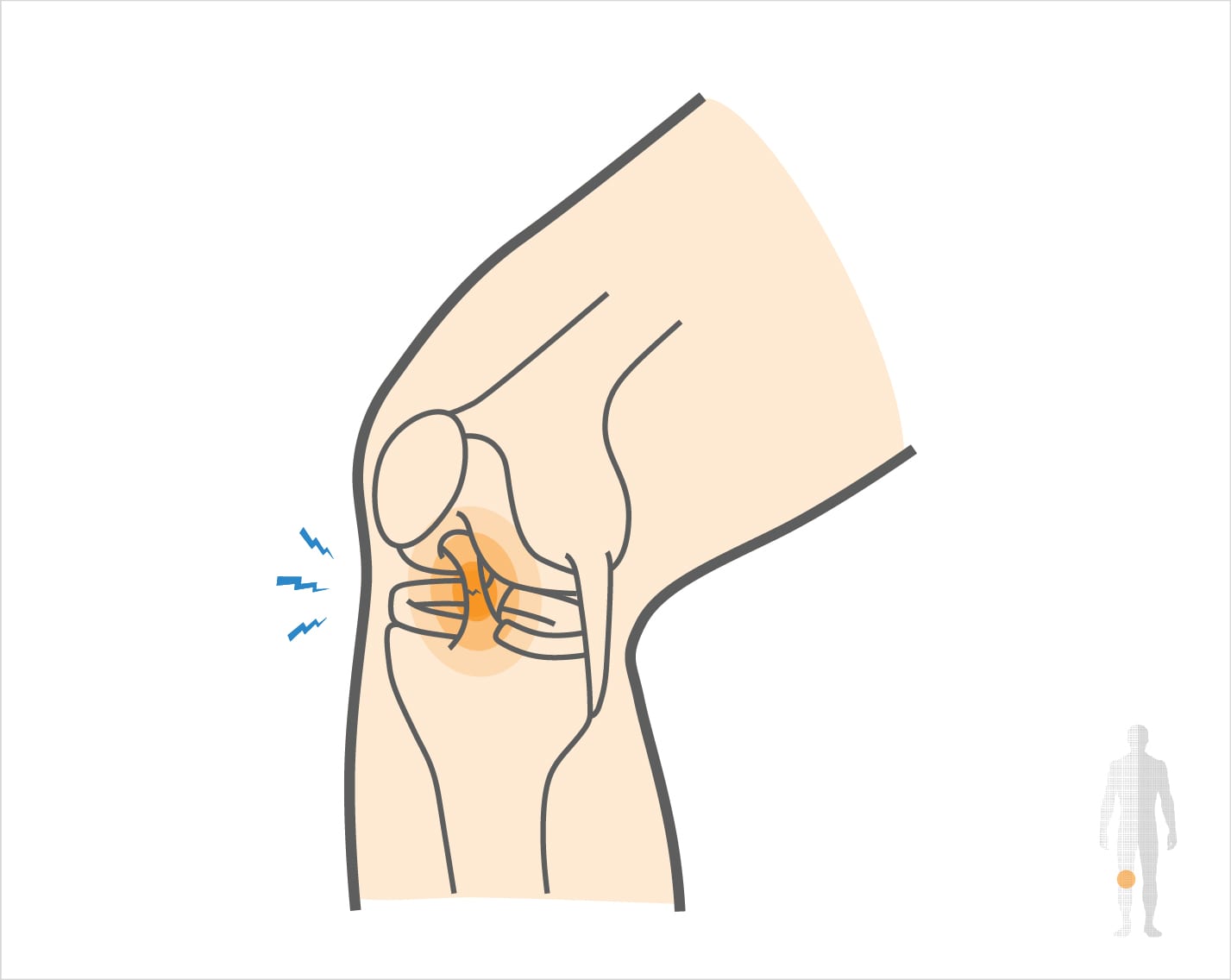
The anterior cruciate ligament (ACL) is important for maintaining stability of the knee joint, particularly in activities involving weaving, pivoting or kicking. The knee becomes unstable with a ruptured ACL and the joint may become more damaged over time. ACL reconstruction is the surgical treatment of choice to restore stability at the knee joint. ACL reconstruction is surgery to replace a torn anterior cruciate ligament (ACL) — a major ligament in your knee. ACL injuries most commonly occur during sports that involve sudden stops and changes in direction — such as soccer, football, basketball and volleyball. Ligaments are strong bands of tissue that attach one bone to another bone. During ACL reconstruction, the torn ligament is removed and replaced with a band of tissue that usually connects muscle to bone (tendon). The graft tendon is taken from another part of your knee or from a deceased donor.
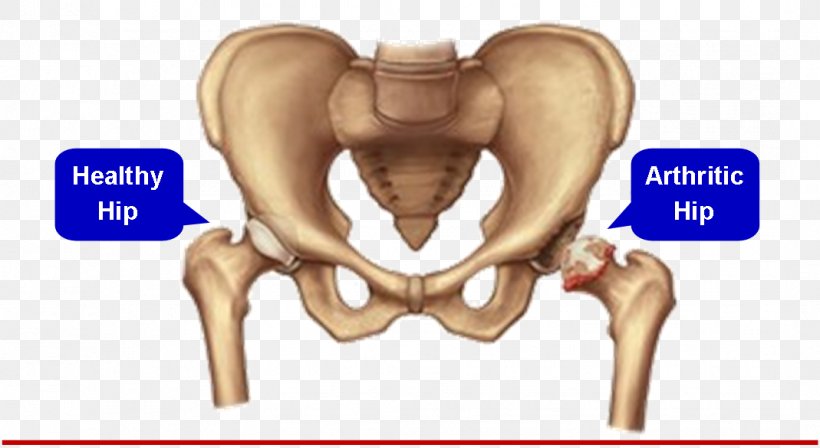
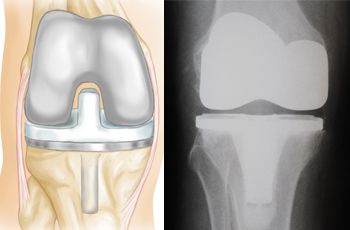
Total joint replacement is a surgical procedure where parts of an arthritic or damaged joint are removed and replaced with a metal, plastic or ceramic device called a prosthesis or implant. The prosthesis is designed to reproduce the shape and motion of the normal joint. During hip replacement, the damaged ball of the hip ball and socket joint is removed and replaced with a metal or ceramic ball that attaches to a stem that fits into the femur. During total knee replacement surgery, a thin amount of bone along the surface of the joint is removed from the end of the femur or thigh bone, the top of the tibia or leg bone, as well as the underside of the kneecap. Hip and knee replacement are two of the most commonly performed operations in orthopedic surgery. Both procedures are very successful at eliminating pain, correcting deformity and improving patient mobility so patients can regain quality of life and get back to the activities they enjoy. During hip replacement, the damaged ball of the hip ball and socket joint is removed and replaced with a metal or ceramic ball that attaches to a stem that fits into the femur. The prosthesis is usually coated with a special material into which the bone will grow over time. In some instances, however, the prosthesis is cemented into the bone. The socket portion of the ball and socket joint is also replaced with a metal cup that is placed into the pelvis. A plastic liner is then snapped into the metal cup and rotates with the new ball on the end of the femoral stem. The prostheses and implants come in a variety of shapes and sizes that can be tailored to the individual. During total knee replacement surgery, a thin amount of bone along the surface of the joint is removed from the end of the femur or thigh bone, the top of the tibia or leg bone, as well as the underside of the kneecap. The surfaces of the bone are then shaped with tools and sized to allow an appropriate implant fit for each individual knee. The major ligaments and tendons of the knee are typically kept in place to provide stability and normal motion of the knee joint. Like hip replacements, knee replacements can either be cemented into place or are covered in a special material into which the bone will grow.

Fracture management can be divided into nonoperative and operative techniques. The nonoperative approach consists of a closed reduction if required, followed by a period of immobilization with casting or splinting. Closed reduction is needed if the fracture is significantly displaced or angulated. Pediatric fractures are generally much more tolerant of nonoperative management, owing to their significant remodeling potential. If closed reduction is inadequate, surgical intervention may be required. The goal of fracture management is bony union of the fracture without further bone or soft-tissue damage that enables early restoration of maximal function.Early restoration of function minimizes cardiopulmonary compromise, muscle atrophy, and the loss of functional ROM. It also minimizes impairments associated with limited skeletal weight bearing (e.g., osteoporosis). Fractures are managed either nonoperatively or operatively on an elective, urgent, or emergent basis depending on the location and type of fracture, presence of secondary injuries, and hemodynamic stability. Elective or nonurgent management (days to weeks) applies to stable fractures with an intact neurovascular system or fracture previously managed with conservative measures that have failed. Urgent management (24 to 72 hours) applies to closed, unstable fractures, dislocations, or long bone stabilization with an intact neurovascular system. Emergent management applies to open fractures, fractures/dislocations with an impaired neurovascular system or com¬partment syndrome, and spinal injuries with increasing neurologic deficits. Fracture reduction is the process of aligning and approximating fracture fragments. Reduction may be achieved by either closed or open methods. Closed reduction is noninvasive and is achieved by manual manipulation or traction. Open reduction with internal fixation (ORIF) techniques require surgery and fixation devices commonly referred to as hardware. ORIF is the treatment of choice when closed methods cannot maintain adequate fixation throughout the healing phase. In order to decrease the extent of soft-tissue disruption that occurs when direct reduction is required, minimally invasive surgical techniques for fracture fixation have been developed. In minimal access surgery or minimally invasive surgery (MIS), the surgeon uses the least invasive access portal and mainly indirect reduction techniques to fixate the fracture.
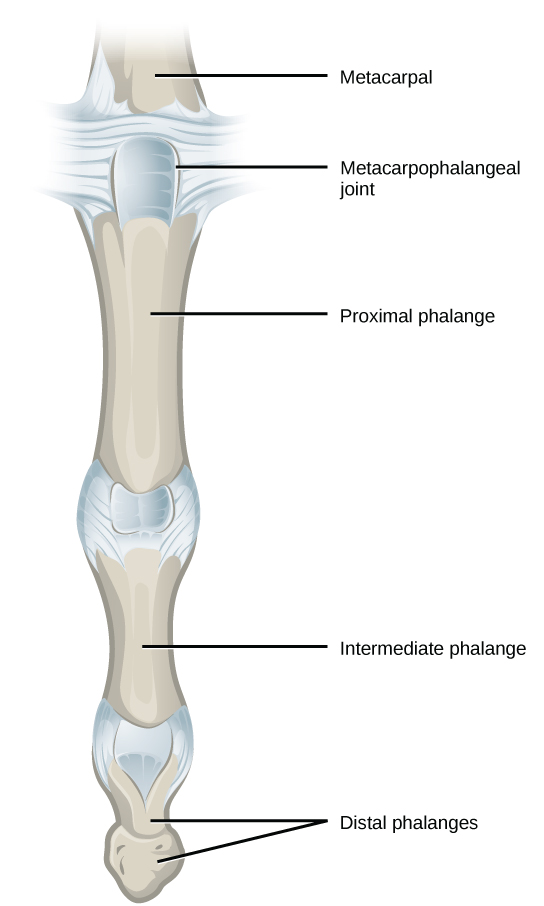
A joint dislocation, also called luxation, occurs when there is an abnormal separation in the joint, where two or more bones meet. A partial dislocation is referred to as a subluxation. Dislocations are often caused by sudden trauma on the joint like an impact or fall. A joint dislocation can cause damage to the surrounding ligaments,tendons, muscles, and nerves. Dislocations can occur in any joint major (shoulder, knees, etc.) or minor (toes, fingers, etc.). The most common joint dislocation is a shoulder dislocation. Treatment for joint dislocation is usually by closed reduction, that is, skilled manipulation to return the bones to their normal position. Reduction should only be performed by trained medical professionals, because it can cause injury to soft tissue and/or the nerves and vascular structures around the dislocation. The sideline clinician has unique challenges treating the athlete with a joint dislocation. Sideline clinicians have limited imaging options to diagnose other injuries and the risk of manipulating an associated fracture while trying to reduce the joint. Similarly, sideline reductions have limited anesthesia available for both patient comfort and facilitation of the reduction if muscle spasm has occurred.Furthermore, there may be limited assistance from non–medically trained individuals attempting to help in a reduction procedure. All of these variables should be considered when caring for the athlete on the sidelines. Despite these limitations, definite reduction and stabilization of joint dislocations can have a significant benefit for the patient by reducing pain and minimizing potential neurovascular compromise. The sideline clinician should be familiar with common dislocations and their reduction techniques. The clinician should weigh the benefits and risks of the reduction based on their comfort level with the reduction and on the presence of associated injuries. It is important that the sideline clinician document a neurovascular examination before and after a joint reduction. Once the reduction has been performed, the athlete needs radiographic confirmation of the successful joint reduction and evaluation for associated injuries.

Optimal management of pediatric orthopedic trauma requires understanding the unique characteristics of the immature musculoskeletal system. The principles of pediatric orthopedic trauma management include anticipating future growth and bone remodeling potential, minimizing physeal injury, and aggressive treatment of open fractures and compartment syndromes. Management of pediatric orthopedic trauma requires understanding the unique characteristics of the immature musculoskeletal system. The principles of pediatric orthopedic trauma management include anticipating future growth and bone remodeling potential, minimizing physeal injury, and aggressive treatment of open fractures and compartment syndromes.


